The use of Non-Invasive Ventilation (NIV) for COVID-19 has been an area of great controversy – see our COVID-19 ED Assessment & Management Guideline, in the Oxygenation Overview and NIV & HFNC sections for full details. Early in the pandemic when the “early intubation” approach was prominent, many guidelines recommended against NIV due to concerns regarding risk of infectivity to staff (being an Aerosol Generating Procedure (AGP)) and possible lack of utility in avoiding eventual intubation. This approach was a marked deviation from the standard of care approach to hypoxaemic type 1 respiratory failure and this deviation was recommended based on very limited relevant evidence.
Subsequently early experience from the pandemic epicentres has found:
- That the “early intubation” approach appears to be associated with high mortality , high re-intubation rates post extubation and prolonged time on ventilators. Various potential reasons for this have been proposed. [see Oxygenation Overview section]
- CPAP to be a a useful therapy for patients who remain hypoxaemic despite high flow oxygenation provided via a non-rebreather mask and has been effective in avoiding intubation (see Oxygenation Overview section). Additionally, initial concerns re high infective risk to staff have been ameliorated by the use of newer ventilators with closed-circuit systems and viral filters with staff wearing Tier 2 PPE indicated for AGPs and appropriate patient room selection. [See NIV & HFNC section]
While CPAP is broadly recommended, BiPAP/Bi-level NIV appears to have a limited role. True respiratory fatigue with hypercapnoea (type 2 respiratory failure) is apparently quite uncommon in COVID-19 and some sources still recommend that these patients proceed to early intubation rather than use BiPAP unless the patients have BiPAP responsive co-morbid presentations such as acute exacerbations of COPD.
Updated Guideline Recommendations on NIV:
- Australia: National COVID-19 Clinical Evidence Task Force: Caring for patients with COVID-19 (Updated 30/4/20)
- “…consider using NIV therapy for patients with hypoxaemia associated with COVID-19, ensuring it is used with caution and strict attention is paid to staff safety.”
- US: National Institute of Health Coronavirus Disease 2019 (COVID-19) Treatment Guideline (released 21/4/20)
- “In the absence of an indication for endotracheal intubation, the Panel recommends a closely monitored trial of NIPPV for adults with COVID-19 and acute hypoxemic respiratory failure for whom HFNC is not available.”
- UK: NHS – Guidance for the role and use of non-invasive respiratory support in adult patients with COVID-19 (confirmed or suspected) version 3, (Updated 6/4/20)
- “CPAP is the preferred form of non-invasive ventilatory support in the management of the hypoxaemic COVID-19 patient…”
HFNC also endorsed
While there were mixed recommendations early in the pandemic, more sources have since come out in favour of the use of High Flow Nasal Cannula (HFNC). There are several potential advantages of using HFNC before NIV [see NIV & HFNC section] which has resulted in the former often being suggested to be trialled before the latter, as part of a graded respiratory support strategy. The NIH 21/4/20 guideline explicitly recommends this and the NC19CET 30/4/20 guideline implicitly favours HFNC over NIV by recommending to “use” HFNC and “consider use” of NIV. The NHS 6/4/20 guideline argues against HFNC partly due to concerns re consumption of oxygen supplies.
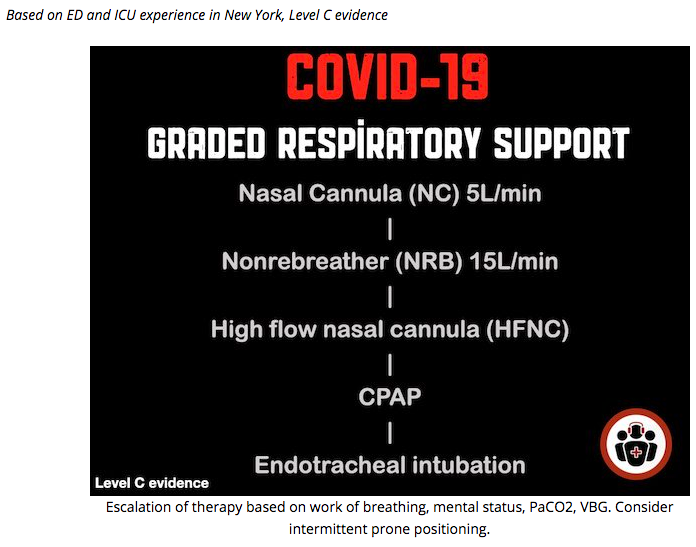
Suggested graded respiratory support progression from EM Cases COVID-19 Updates 5/4/20
The “Early Intubation” approach is dead … or at least “modified”
The effect of these guideline updates is that while the “early intubation” approach has been effectively dead for a couple weeks now, these guideline updates practically have the effect of burying it, at least until more rigorous data becomes available.
The only caveat is that a “modified early intubation” approach may still arguably be warranted:
- To prevent P-SILI (Patient Self Induced Lung Injury);
- Where a patient is not achieving a significant reduction in work of breathing from a limited trial of HFNC or NIV (e.g. 1-2 hours), it has been suggested that such patients should be considered for “early intubation” rather than persist with prolonged periods of ineffective non-invasive therapies. This “modified early intubation strategy” is thought to prevent Patient Self Induced Lung Injury (P-SILI) from excessive tidal volumes and intra-pleural pressure swings which may convert type L phenotype patients to the presumed higher mortality type H patients. [see Oxygenation Overview section]
- In the uncommon patients with hypercapnoea, except perhaps acute on chronic COPD patients who could trial BiPAP (see above).
- In patients with abnormal mentation
Clarifying early intubation: Note that while “intubating early in the disease process” is no longer advised, “making early decisions regarding intubation” when evaluating trials of NIV and HFNC is subtly different and definitely advisable. The COVID-19 intubation process takes significant time to prepare and execute and given patients can deteriorate quickly, failure to decide to intubate early could result in patient demise. This reinforces the above recommendation to not persist with prolonged trials of non-invasive therapy that are ineffective at achieving clinical targets, such as reduced work of breathing with normal mentation.
Lower the PEEP and increase the FiO2
There is also an emerging belief that high PEEP strategies may also increase lung injury and mortality by converting type L phenotype patients to type H and consequently CPAP with low to intermediate PEEP only (e.g 5-10cm H20) or HFNC (which provides such low PEEP by design) have been advocated to maximise benefit and minimise harm. [see Oxygenation Overview section].