Contents
Tip: Perform the HINTS+ Exam in Reverse Order
HINTS+ Peripheral – What findings confirm a peripheral cause of AVS
Understanding the Head Impulse Test & the Vestibular-Ocular Reflex (VOR)
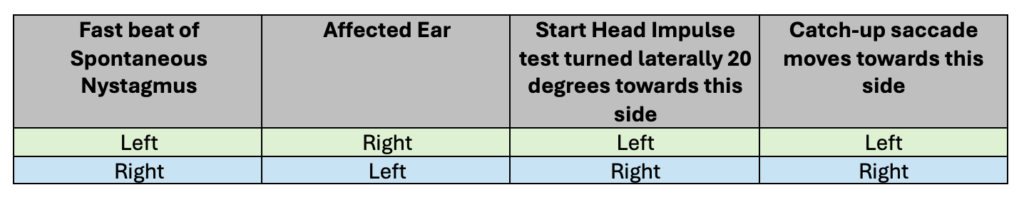
Table summarising relationship between direction of nystagmus, affected ear and catch-up saccade

Purpose of the HINTS+ Exam
The HINTS+ exam should only be performed in patients with AVS (Acute Vestibular Syndrome) with associated spontaneous nystagmus at rest who lack red flags for a central cause on prior neurological assessment. Such patients generally have a peripheral cause of their AVS (peripheral AVS – usually vestibular neuritis) but occasionally can have a central cause (central AVS) such as posterior circulation stroke.
Therefore the purpose of the HINTS+ exam is to safely confirm that such patients are indeed suffering from a peripheral cause of AVS without any further investigation.
Note this refers to the strict definition of AVS, which is a very distinct clinical entity representing AVS with both continuous dizziness (usually but not always described as a vertigo like sensation) and spontaneous nystagmus present at rest, associated with postural instability and usually nausea and/or vomiting. As explained in our section below (Understanding the Head Impulse Test and the VOR), the presence of spontaneous nystagmus is critical to understanding and applying the HINTS+ exam. For the purposes of this article, AVS adhering to this strict definition that requires the presence of spontaneous nystagmus will be described as “true-AVS”.
Almost all patients with peripheral AVS have spontaneous nystagmus present in the first few days. As such AVS patients without spontaneous nystagmus (that will be described as pseudo-AVS in this article), represents a different clinical entity within which the Head Impulse testing part of the HINTS+ exam has not been validated and should not be used. Using it in this group will reliably fail to confirm a peripheral cause and will falsely create concern for a central cause.
See the detailed partner article, “Approach to Dizziness & Vertigo” for more information, in particular the AVS section.
What is the HINTS+ Exam
[Please note that useful videos demonstrating the HINTS+ exam and tips for performing it are provided at the end of this article.]
The HINTS+ (HINTS plus) exam consists of
- Head Impulse (HI) testing (explained in detail below)
- Nystagmus
- First confirming the presence of spontaneous nystagmus that is consistent with peripheral AVS – horizontal +/- torsional (rotatory) component – as it is a precursor and prerequisite to the performance of the Head Impulse test part of the HINTS+ exam.
- Patterns of nystagmus that indicate a central cause are vertical or “pure torsional” (as opposed to horizontal with a torsional component)
- Tip: Spontaneous nystagmus can be suppressed by visually fixating on a point. If you suspect peripheral-AVS but can not see spontaneous nystagmus, try Dr Peter John’s “blank paper” trick, which can reveal spontaneous nystagmus by removing fixation. Alternatively, if available, the more expensive Frenzel goggles can be used for the same purpose.
- Second: Test Gaze-Evoked Nystagmus
- The patient is asked to look side to side about 30 degrees from midline to confirm that horizontal nystagmus they have is indeed consistent with a peripheral cause – i.e. it is unidirectional nystagmus, where the fast beat of the nystagmus always beats in one direction regardless of whether the patient is looking left or right.
- If bidirectional horizontal nystagmus is present (fast beat to right when looking right and fast beat to left when looking left) this suggests a central cause.
- Avoid testing at the extremes of gaze or you may detect the normal end-gaze nystagmus and confuse this for the pathological bidirectional nystagmus (see Pitfalls below)
- First confirming the presence of spontaneous nystagmus that is consistent with peripheral AVS – horizontal +/- torsional (rotatory) component – as it is a precursor and prerequisite to the performance of the Head Impulse test part of the HINTS+ exam.
- Test of Skew
- To detect any vertical skew deviation with the cover-uncover eye test.
- Vertical skew deviation is diagnosed, if upon removing the hand covering one eye, the eye uncovered moves in a vertical direction (either vertical or diagonal, but not pure horizontal movement).
- Vertical skew deviation has a low sensitivity but high specificity for detecting a central cause of AVS.
- + (plus) – represents a quick gross test of hearing by rubbing your fingers together next to each ear and comparing their hearing.
- Testing hearing was added later as an afterthought as the “+” because the original HINTS exam didn’t include it.
- It was included to detect AICA (Anterior Inferior Cerebellar Artery) stroke that can cause AVS with unilateral reduction in hearing. Interestingly while labrynthitis (inflammation of both vestibular and cochlear components of the 8th cranial nerve), a peripheral cause, can also cause hearing loss this is actually a very uncommon peripheral cause of AVS. Vestibular neuritis, inflammation of only the vestibular nerve, accounts for the vast majority of peripheral AVS cases). Consequently new hearing loss sufficiently raises the relative probability of a central cause to warrant investigation.
Key Tip: Perform the HINTS+ Exam in Reverse Order
- Tip: An easy mental strategy to avoid performing the Head Impulse test on the wrong patient is to perform the HINTS+ exam in the reverse order of the acronym so that the Head Impulse test is the last part of the examination, only performed if appropriate “peripheral” findings exist on the prior parts of the examination. So the order would be:
- “+” – assess hearing
- Test of Skew
- Nystagmus
- Head Impluse testing – performed only if appropriate findings on the above tests.
- Rationale:
- The Head Impulse test should only be performed to confirm a strong suspicion of peripheral AVS based on:
- 1) The absence of Red Flags for a central neurological cause and
- 2) The patient has spontaneous nystagmus that is consistent with a peripheral cause (horizontal +/- torsional component) where the fast beat does not change in direction on gaze testing.
- Most neurological red flags for a central cause are ruled out at Step 1 of the Approach to Dizziness and Vertigo. Additional red flags are ruled out as part of the HINTS+ exam – loss of hearing, vertical skew deviation and a central nystagmus patterns (spontaneous vertical/pure torsional or directional changing horizontal nystagmus on gaze testing).
- Thus, performing the HINTS+ exam in reverse order, ensures the Head Impulse test is only performed on appropriately qualifying patients.
- Note that there is no major harm of assessing hearing, test of skew and nystagmus testing in any dizzy patient. In fact arguably one could choose to assess these feature as part of a general neurological assessment in Step 1 and unlink this from the Head Impulse testing entirely – the only downside of this would be loss of the memorable HINTS+ acronym and consequent risk of forgetting aspects of the exam.
- However there is clear harm in performing the Head Impulse test on the wrong patient by:
- Falsely confirming peripheral AVS in a person with red flags for a central cause
- Falsely indicating a central cause warranting unnecessary hospital admission and investigation by performing the Head impulse test in a patient without spontaneous nystagmus.
- Performing the HINTS+ exam in reverse order prevents this from happening.
- The Head Impulse test should only be performed to confirm a strong suspicion of peripheral AVS based on:
“HINTS+ Peripheral” – What findings confirm a peripheral cause of AVS?
In patients with true-AVS, if red flags for a central cause have already been excluded at Step 1 of the Approach to Dizziness & Vertigo, then the following combination of findings reliably indicates a person with a peripheral cause of their AVS (usually vestibular neuritis):
- No vertical skew deviation
- No new hearing deficit
- Spontaneous horizontal nystagmus (+/- torsional component) that is undirectional on gaze testing.
- Head impulse test that is positive for a unilateral catch-up saccade in the same direction as the fast beat of their spontaneous nystagmus (explained in detail below).
Note that all findings are required to comfortably confirm the already suspected diagnosis of peripheral AVS, without further investigation – if any of the above are not present, the patient should generally be investigated for a central cause.
Pitfalls of the HINTS+ Exam
There are 2 main pitfalls of the HINTS+ exam.
1. Mistaking End-Gaze Nystagmus for bidirectional nystagmus
Bidirectional nystagmus, where the fast beat changes direction when the gaze is moved from one side to the other is strongly suggestive of a central cause of AVS. However this can be easily confused with the very normal end-gaze nystagmus, which is nystagmus seen at the extremes of gaze that is low amplitude and non-sustained (lasts for a few beats). When looking to the left extreme, nystagmus beats to the left and the opposite occurs when looking right. This video demonstrates end-gaze nystagmus, how to recognise it and stop it from occurring. In short, only examine gaze-evoked nystagmus out to 30 degrees each way and if you suspect end-gaze nystagmus, bring the gaze a little back towards the midline to see if it disappears.
2. Failing to detecting the catch-up saccade on Head Impulse testing
The main well recognised problem with the HINTS+ exam is that the HI test can be tricky to perform without proper understanding and practice. Consequently this can result in failing to observe the catch-up saccade, and thus incorrectly diagnosing a central cause of AVS, initiating unnecessary admission and investigation. Studies show that it is often performed both poorly and in the wrong patients (e.g. pseudo-AVS) by emergency clinicians but that this can be improved with specific training. This article seeks to address this training need by providing a better understanding of the pathophysiology underlying peripheral AVS and tips to performing optimal HI testing so that you do not miss that catch-up saccade.
Understanding the Head Impulse test & the Vestibular-Ocular Reflex
To understand the Head Impulse (HI) test, exactly how to perform it and why it should only be performed on patients with continuous spontaneous nystagmus at rest, it is useful to review the vestibular ocular reflex (VOR) between the vestibular apparatus (semicircular canals of the inner ear), the brainstem and our eyes. The VOR keeps our eyes fixed on a target despite head movements. If we fix our gaze on a target, and move our head to one side, the VOR will reflexively move our eyes in the opposite direction.
The signals from our vestibular apparatus are usually in balance. When we turn our head to the left, the left side is stimulated and the right inhibited which causes our eyes to move to the right (and vice versa) to maintain fixation on the target.
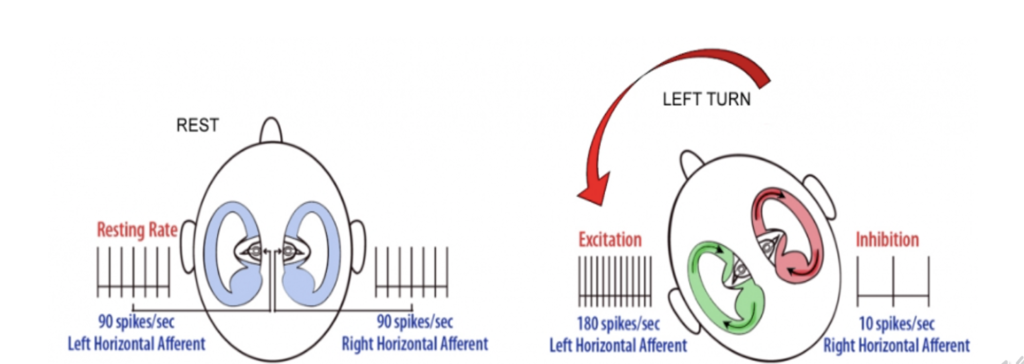
When a patient has vestibular neuritis their vestibular system on one side is dysfunctional (suppressed). So for example, if we have right sided vestibular neuritis, the right vestibular signals are suppressed. This creates an relative imbalance such that the signals from the left side are now greater than the right. This erroneously activates the VOR based on a false perception that that the head is turning to the left (the usual cause of left side signals being more active than right side), so the eyes slowly move to the right (slow phase of nystagmus). Upon realising the eyes are now misaligned with the target, the brain corrects the eyes back the other way (the left) which represents the fast beat of the nystagmus. Importantly, as the right ear vestibular signals are continuously suppressed, this creates continuous spontaneous nystagmus of slow phase to the right (inappropriate VOR activation) and fast beat to the left (brain correction for this). The opposite is of course true for left sided vestibular neuritis.
So the fast beat of nystagmus points away from the affected ear.
Enter the Head Impulse Test.
Ask the patient to fix their gaze at all times on a central point (e.g. your nose or a smartphone). If the fast beat of the spontaneous nystagmus is to the left then, as in the above example, the affected side is the right. So start with the head turned laterally 20 degrees to the left. Then rapidly turn the head to the midline which is towards the right, affected ear. By rapidly turning towards the right, this overwhelms the dysfunctional right vestibular system. It is unable to increase its activation to successfully trigger the VOR. So instead of the eyes remaining fixed on the target they follow the head movement to the right and having passed the target, a split second later will try and correct and move back towards the midline – to the left. This correction at the end is the diagnostic “catch-up saccade” and is in the same direction as the fast beat of the spontaneous nystagmus – both are away from the affected ear.
The Head Impulse test should only demonstrate this catch up saccade when tested in one direction, so test both sides several times to be sure that this is the case.
Critically the cerebellum is not involved in the VOR, which is why it is preserved in central causes of AVS. Hence a “normal” HI test, where a unilateral catch-up saccade is not detected can be indicative of a central cause when HI testing is appropriately performed only on patients with “true-AVS” (present spontaneous nystagmus that is unidirectional).
In summary
- Peripheral AVS such as vestibular neuritis causes dysfunction of a unilateral vestibular system (left or right ear).
- This erroneously activates the VOR as if the head was moving away from the affected ear (even though it isn’t) so the eyes are moved slowly (slow phase of nystagmus) towards the affected ear.
- This results in a rapid correction afterwards back to the other way – i.e. the fast beat of nystagmus is away from the affected ear.
- HI test should be performed by starting the head laterally turned 20 degrees towards the same direction as the fast beat of the spontaneous nystagmus (away from the affected ear), then rapidly turning to the midline (towards the affected ear).
- The eyes will follow the head and overshoot towards the affected ear, followed by a catch up saccade the other way to correct for this.
- So the catch up saccade will be in the same direction as the fast beat of the nystagmus.
- Repeat testing several times in both directions (always rapidly turning towards the midline) in order to confirm the catch-up saccade is only occurring when turning the head in one direction (the same direction as the fast beat of the nystagmus, away from the affected ear).
Which ear does the nystagmus in vestibular neuritis beat towards?
(VOR and the Head Impulse Test also demonstrated in this video)
Table
Relationship between direction of nystagmus, affected ear and catch up saccade in Head Impulse testing in peripheral AVS
Tips for Performing the Head Impulse test
- First ensure you are only performing this on patients with true-AVS (spontaneous nystagmus present at rest) with red flags for central causes excluded by both general neurological assessment (explained in the Approach to Dizziness & Vertigo article) and by performing the HINTS+ exam in reverse order.
- Have an assistant use a smartphone to record the test (with patient consent) recording the image from nose to mid forehead. It is difficult to both perform and interpret the test simultaneously so it is easier to interpret the recording.
- Determine the direction of the fast beat of the nystagmus. Make a mental note – assuming this is “peripheral” AVS, the affected ear is the opposite side.
- Start the HI test with head turned 20 degrees laterally towards the same direction as the fast beat. (e.g. if fast beat is towards the left, start with head turned to the left, away from the affected ear)
- Rapidly turn their head to the midline – turning in the opposite direction to their nystagmus fast beat – towards the affected ear to overwhelm its vestibular system (e.g if left beating nystagmus, turn rapidly right towards the midline).
- Look for the catch-up saccade going back the other way
- i.e catch-up saccade moves in the same direction as the fast beat of the nystagmus (away from the overwhelmed affected ear)
- Repeat the test, starting on the other side to confirm you don’t see a catch up saccade on that side. In patients with peripheral AVS (usually vestibular neuritis), the HI test should only be positive when testing one side.
- Be unpredictable:
- In actual practice, one should perform the test several times on both left and right sides in a random fashion. Gently and slowly laterally rotate the head in each direction 20 degrees away from midline repeatedly, and then unpredictably turn it back rapidly towards the midline – this represents one single “test”. Repeat this process several times. This is so the patient can’t predict when, and in which direction, you will rapidly turn to the midline. If they can mentally predict it, conscious eye control can track the target and compensate for a failing VOR and you will not see a catch up saccade resulting in a false diagnosis of a central cause.
- Always turn rapidly towards the midline, rather than turning rapidly away from the midline – not only is this the correct way to identify the catch-up saccade, it also helps prevent turning the head too far laterally and causing injury to the neck.
Useful HINTS+ Exam Videos
HINTS+ Exam Quick Review
Tips for Performing the HINTS+ Exam